When plans were announced in 2011 to create an integrated community clerkship program in Trail, the idea was embraced by both the medical community and the public. As with most rural BC communities, physician recruitment and retention remains an ongoing challenge, but one which the program was designed to help address.
The Trail ICC program admits two third year students annually for a full year of in-depth clinical training. Each student is matched with two primary family practice preceptors working collectively to care for patients in the clinics and in addition to training alongside specialists at Kootenay Boundary Regional Hospital.
“The creation of this program is a remarkable acknowledgement that education can be delivered as well and as effectively in a small, rural community as in a larger urban centre.” says Dr. Cheryl Hume, family physician and ICC site director. “It validates the skill set of those working here, creates a greater culture of medical education, and ultimately improves quality of care for patients.” Dr. Hume also attributes the effective partnership with the Interior Health Authority for supporting the program’s success.
Patient continuity is a key strength of the ICC program as students are involved from the initial visit at the family practice clinic, through their treatments with specialists, and right back to follow-up. “You are able to make a lot of connections based on family history and get a real breadth of procedures,” says Dr. Libby McCoid, family physician. “We are showing the students the different relationships patients have with their family doctor versus specialists.”
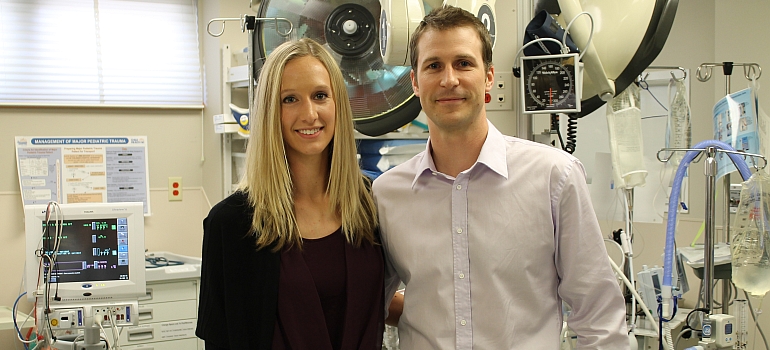
Third year medical students Alexander Ednie and Katie Eddy, who entered medical school as a couple, have spent the past ten months as the only two learners in the community and the hospital. “As you get to know more family practice patients, it’s nice because you know their history and what treatments they have been going through,” says Ednie. “You also get a ridiculous amount of hands-on experience and exposure to your fields of interest because the physicians know you and what you are capable of,” says Eddy.
The integrated model rotates the students through eight different clinical specialties ranging from emergency medicine to surgery to psychiatry divided over the course of the year. “You really get to see the evolvement of the students rather than just seeing them for a couple of weeks,” says Dr. Tara Gill, emergency physician. “You get to see where they are at in the beginning, be involved with the teaching, and move on with them throughout the year.”
An impressive team of 60 physicians are involved with teaching in the program. Some are relatively new to clinical teaching, whereas others like Dr. Ron Cameron are provided with a renewed link to medical education. “Getting involved with teaching at a smaller site has provided a balance again of being connected to the academic,” says Dr. Cameron, general surgeon. “Teaching really forces you to focus on your own practice and have a critical look at why you are doing things when having to justify it to the students.”
For Ednie and Eddy, their collective experience has been one they will never forget and has only fueled their passion to practice rural medicine in the future. “If we were to graduate from our program and an opportunity came up in Trail, we would come back in a heart beat,” adds Ednie. “The staff, physicians, everybody – it’s such a cohesive environment.”
The Trail ICC program will welcome two new students this September. Based on the program’s success, potential expansion in the number of students is being reviewed for the following academic year.