Projects will look at improving N95 masks, mental health and well-being
The BC Ministry of Health is investing in BC Interior research universities to understand the harmful effects of COVID-19 and mitigate its impact on communities across the province.
The province has funded five collaborative research projects through the Interior University Research Coalition (IURC), a partnership between Thompson Rivers University (TRU) in Kamloops, the University of British Columbia, Okanagan (UBCO) in Kelowna and the University of Northern British Columbia (UNBC) in Prince George.
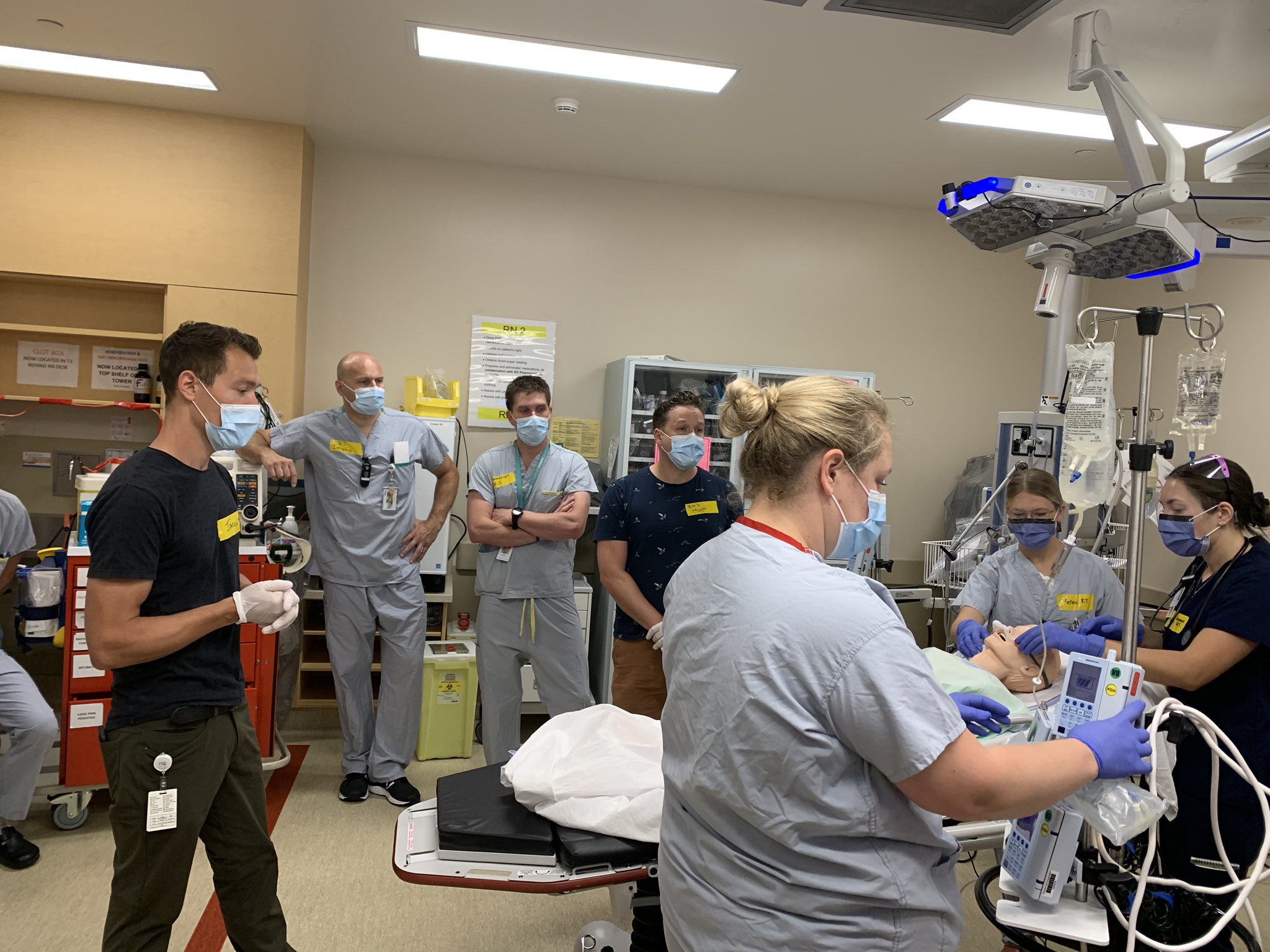
The projects being funded range from identifying the effects of the pandemic on the mental health and well-being of people living in rural communities to developing telehealth programs that will engage older adults outside urban centres. Other projects include a focus on improving the lifespan of N95 masks, as well as building a better understanding of whether new technologies are improving the resiliency of rural health-care practitioners.
“This is a win-win-win situation for the province, for the universities, and for the communities we serve in terms of the impact this research will have on the health and quality of life for the people who live there,” says Will Garrett-Petts, associate vice-president, research and graduate studies at TRU.
He adds that the IURC has developed a model that can ensure responsible and innovative research.
“The work we’re doing is meaningful and is guided by the interests of the local and regional communities,” he says. “This is a wonderful model of collaboration, and one we are collectively celebrating.”
UBC Okanagan’s Vice-Principal and Associate Vice-President for Research and Innovation Phil Barker agrees. He says his campus is especially excited to be working on an initiative that is highly collaborative and that spans campuses and institutions across the BC interior.
“We’re delighted that the BC Ministry of Health is investing in this initiative to help mitigate the effects of COVID-19 throughout our province,” explains Barker. “Our researchers have been able to mobilize quickly through the tri-university partnership and each of the selected projects will leverage our respective strengths to serve communities across BC.”
The BC Ministry of Health has provided the IURC with $150,000 to launch this initiative. The IURC was established in 2017 to advance the research and innovation capacity and commercialization potential of the BC Interior and create new opportunities for economic and social innovation. The inaugural funding is focused largely on COVID-19 issues that affect the BC Interior but the results from these projects will help support regional and provincial health care decision-making and provide real-world opportunities for students to gain experience in the complex, ever-changing realm of health care.
“When researchers from different institutions collaborate across disciplines, the research outcomes benefit from different perspectives and synergies that result from cross-institutional collaboration,” says Kathy Lewis, acting vice-president of research at UNBC. “These projects are fantastic examples of what’s possible when researchers from across the BC Interior come together and seek solutions to pressing public health concerns.”
About the projects
- Shannon Freeman, associate professor in UNBC’s School of Nursing, has partnered with Piper Jackson, assistant professor of computer science at TRU, to develop a COVID-19 risk assessment tool that identifies homecare clients who are at greatest risk of contracting the virus.
- Jian Liu and Abbas Milani of UBCO’s School of Engineering will be working with Hossein Kazemian of UNBC to improve the lifespan of nanofibres and activated carbon mats in N95 masks.
- Brodie Sakakibara, assistant professor in UBCO’s Southern Medical Program and investigator in the Centre for Chronic Disease Prevention and Management, is working with researchers at UBCO, UNBC and Interior Health to create a student-delivered Community Outreach Telehealth Program that will engage older adults from outside urban centres and establish best practices for providing health support during a pandemic.
- TRU’s Bala Nikku has teamed up with Khalad Hasan from UBCO and Rahul Jain from UNBC to better understand whether new technologies are improving the resiliency of rural health care practitioners.
- Nelly Oelke, associate professor in UBCO’s School of Nursing and scientific director of the Rural Coordination Centre of BC, will be collaborating with UBCO’s Donna Kurtz, UNBC’s Davina Banner-Lukaris and TRU’s Bonnie Fournier to expand ongoing research that explores the mental health impacts of climate change events. The new study will identify the effects of the pandemic on the mental health and well-being of people living in rural communities to help foster resilience.
- Interior University Research Coalition
- The University of British Columbia, Okanagan campus
- Thompson Rivers University
- University of Northern British Columbia
About UBC's Okanagan campus
UBC’s Okanagan campus is an innovative hub for research and learning founded in 2005 in partnership with local Indigenous peoples, the Syilx Okanagan Nation, in whose territory the campus resides. As part of UBC—ranked among the world’s top 20 public universities—the Okanagan campus combines a globally recognized UBC education with a tight-knit and entrepreneurial community that welcomes students and faculty from around the world in British Columbia’s stunning Okanagan Valley.
To find out more, visit: ok.ubc.ca