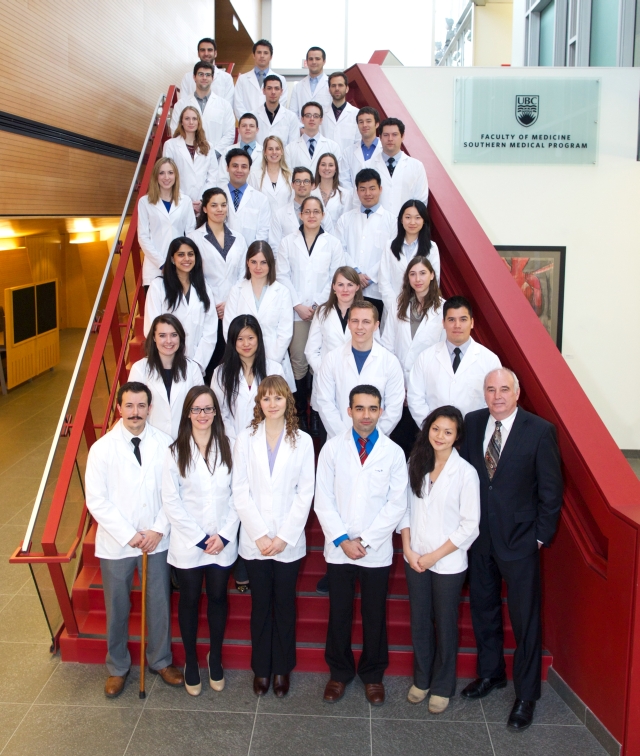
First-year Southern Medical Program students tour the Sensisyusten School as part of the Westbank First Nation visit.
As part of the MD curriculum’s Doctor, Patient, and Society (DPAS) course, students are asked to establish an initial relationship with a local Aboriginal community. Students gain a deeper understanding of Aboriginal health perspectives, the resources available within the community and hospitals, and some of the challenges faced in accessing care that reflects their cultural beliefs.
First-year students were recently welcomed by the Westbank First Nation for a presentation and tour of the band’s health and educational facilities. Presenters included Jayne Taylor and Diana Moar, Aboriginal Patient Navigators, Lloyd Main, Manager, Community Integrated Health Services all with Interior Health and Barbara Coble, Senior Research, Intergovernmental Affairs, Westbank First Nation.
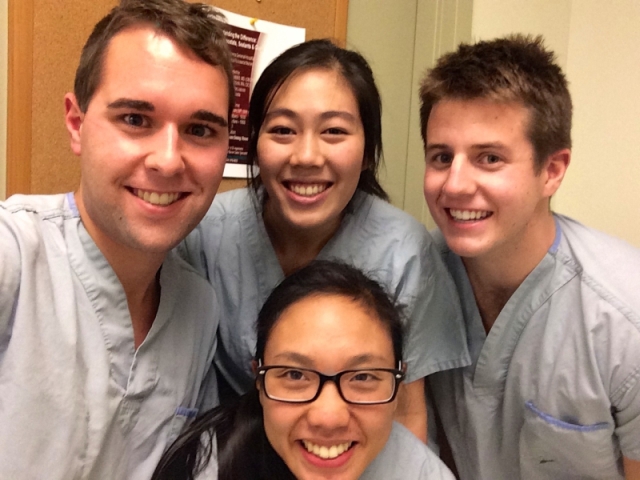
We asked Lucy Shen (LS), first-year SMP student and DPAS course representative about her experience.
Q: What did you learn about Aboriginal health and what were the primary takeaways?
LS: I really enjoyed the content of the presentations as well as the passion the speakers brought. The case studies and stories of the speakers’ own encounters taught us some of the challenges the Aboriginal community may encounter when dealing with the healthcare system.
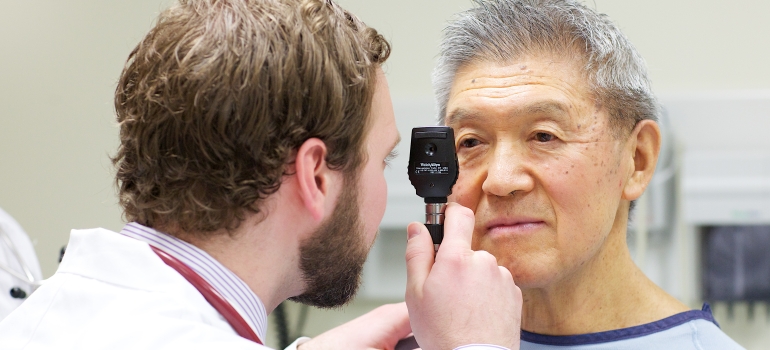
One of the key messages I took away was to be aware of the historical context from which Aboriginal patients emerge. There are many factors in the patients’ lives we don’t know and may not be able to fully understand. However, these are crucial to the patients’ wellbeing and interactions with the healthcare system. We must take the time to support and work with our patients to ensure they receive the best care that they deserve.
An important related message was to reach out to community resources such as the Aboriginal Patient Navigators (APN). In fact, one should be encouraged to engage in any resources that would make your patients’ experiences more comfortable. The APNs provide an invaluable service to ensure Aboriginal patients are able to navigate the healthcare system in an appropriate and timely manner as well as receive continual support in the community.
Q: How does visiting an Aboriginal community impact your learning?
LS: It was really a privilege to be able to visit the Aboriginal community. We saw an abundance of the community’s heritage and culture. Like the presentations, it helped us gain an appreciation and understand a little more about the individual contexts of the Aboriginal patients.
Q: Did the site visit help build any connections with the Westbank First Nation?
LS: Yes! A group of us are very interested in starting a DPAS project with the Westbank First Nation community. Side note: Thank you so much to the Westbank First Nation staff who welcomed us! They were amazing!! We cannot express enough thanks for talking to us and giving us the tour. This is just a first step but a very much needed step towards building community relations.